Alipogene tiparvovec
| |||||||||||||||||||||||||||||
Read other articles:
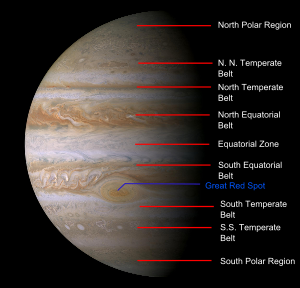
Pola awan di Jupiter tahun 2000 Atmosfer Jupiter adalah atmosfer keplanetan terbesar dalam Tata Surya. Atmosfernya sebagian besar terbentuk dari hidrogen molekuler dan helium dalam proporsi solar yang lebih kurang sama; senyawa kimia lainnya hanya ada dalam jumlah kecil dan meliputi metana, amonia, hidrogen sulfida, dan air. Meskipun air diduga berada jauh di dalam atmosfer, konsentrasi terukur langsungnya sangat rendah. Nitrogen, sulfur, dan gas mulia melimpah dalam atmosfer Jupiter melebihi...

Sebuah kanstin jalan dengan nama jalan di trotoar di New Orleans Kanstin atau pembatas trotoar adalah suatu tepi tempat trotoar yang ditinggikan atau median jalan/reservasi tengah bertemu dengan jalan atau jalan raya lainnya. Sejarah Meskipun kanstin telah digunakan sepanjang sejarah modern, dan memang ada di Pompeii kuno, [1] konstruksi dan penggunaannya secara luas baru dimulai pada abad ke-18, sebagai bagian dari berbagai gerakan menuju keindahan kota yang diupayakan pada periode t...

MarudoKomuneComune di MarudoNegara ItaliaWilayahLombardyProvinsiProvinsi Lodi (LO)Luas • Total4,2 km2 (16 sq mi)Populasi (Dec. 2004) • Total1.202 • Kepadatan29/km2 (74/sq mi)Zona waktuUTC+1 (CET) • Musim panas (DST)UTC+2 (CEST)Kode pos26866Kode area telepon0371 Marudo adalah komune yang terletak di distrik Provinsi Lodi, Italia. Kota Marudo memiliki luas sebesar 4.2 km². Marudo pada tahun 2004, memiliki pendud...

العلاقات الألمانية الكمبودية ألمانيا كمبوديا ألمانيا كمبوديا تعديل مصدري - تعديل العلاقات الألمانية الكمبودية هي العلاقات الثنائية التي تجمع بين ألمانيا وكمبوديا.[1][2][3][4][5] مقارنة بين البلدين هذه مقارنة عامة ومرجعية للدولتين: وجه ال...

Kuća Cveća, mausoleum Josip Broz Tito. Pusara Josip Broz Tito. Nisan pusara Josip Broz Tito. Pemakaman Josip Broz Tito, Presiden Yugoslavia, diselenggarakan pada tanggal 8 Mei 1980, empat hari pasca-kematiannya. Upacara pemakamannya dihadiri oleh banyak negarawan di dunia, baik dari negara-negara Blok Barat, Blok Timur, maupun non-blok, dalam suasana Perang Dingin.[1] Berdasarkan banyaknya politikus dan perwakilan negara yang hadir, upacara pemakaman kenegaraan ini masih dianggap s...

BG Pathum United บีจี ปทุม ยูไนเต็ดNama lengkapBangkok Glass Pathum United Football ClubJulukanThe Rabbits (กระต่ายเเก้ว)Nama singkatBGPUBerdiri2006; 18 tahun lalu (2006)StadionStadion LeoThanyaburi, Pathum Thani, Thailand(Kapasitas: 16,014)PemilikBoon Rawd BreweryKetua Pavin BhirombhakdiManajer Surachai JaturapattarapongPelatih Thongchai SukkokiAsisten Pelatih Amnaj KaewkiewLigaLiga 1 Thailand2022-23ke-9Situs webSitus web resm...

Cet article est une ébauche concernant un coureur cycliste néerlandais. Vous pouvez partager vos connaissances en l’améliorant (comment ?). Pour plus d’informations, voyez le projet cyclisme. Henk NijdamHenk Nijdam en 1964.InformationsNaissance 26 août 1935HarenDécès 30 avril 2009 (à 73 ans)BrédaNationalité néerlandaiseÉquipes professionnelles 1963Peking1964-1965Televizier1966-1967Televizier-Batavus1968Peugeot-BP-Michelin1969Willem II-GazellePrincipales victoires Cha...
Uomo AssorbenteThor con strano l'alleato chiamato l'Uomo Assorbente, disegni di Frenz/Migrom UniversoUniverso Marvel Nome orig.Absorbing Man Lingua orig.Inglese AutoriStan Lee Jack Kirby EditoreMarvel Comics 1ª app.marzo 1965 1ª app. inJourney into Mystery (vol. 1[1]) n. 114 Editore it.Editoriale Corno 1ª app. it.12 ottobre 1971 1ª app. it. inIl Mitico Thor n. 18 Interpretato daNick Nolte (Hulk) Brian Patrick Wade (Agents of S.H.I.E.L.D.) Voci italianePa...
Ираклеониты — ученики гностика Ираклеона (II век). Упоминаются как особая секта Епифанием и Августином; при крещении и миропомазании они соблюдали обряд помазания елеем и при этом произносили воззвания на арамейском языке, которые должны были освободить душу от власт�...

American reality television series American Hot RodBoyd Coddington (r) and his wife Jo sign autographs aboard the nuclear-powered aircraft carrier Nimitz in 2005StarringBoyd CoddingtonCountry of originUnited StatesOriginal languageEnglishNo. of seasons5No. of episodes76ProductionProducerCraig PiligianProduction locationsLa Habra, CARunning time60 minutesProduction companyPilgrim Films & TelevisionOriginal releaseNetworkThe Learning Channel, Discovery ChannelReleaseJanuary 13, 2004 (2...

Hiroshi AoyamaAoyama di Grand Prix Jepang 2009KebangsaanJepangLahir25 Oktober 1981 (umur 42)Ichihara, Chiba, JepangSitus webhiro-aoyama.com Catatan statistik Karier Kejuaraan Dunia MotoGP Tahun aktif2010–2016 PabrikanHonda, BQR, FTR Juara dunia0Klasemen 201625th (1 poin) Start Menang Podium Pole F. lap Poin 70 0 0 0 0 241 Karier Kejuaraan Dunia GP250Tahun aktif2000–2009 PabrikanHonda, KTMJuara dunia1 (2009)Klasemen 20091st (261 poin) Start Menang Podium Pole F. lap Poin 104 9 27 8 11...

Not to be confused with Mid Fife and Glenrothes (Scottish Parliament constituency).Parliamentary constituency in the United Kingdom, 2005 onwards GlenrothesCounty constituencyfor the House of CommonsBoundary of Glenrothes in ScotlandMajor settlementsCardenden, Glenrothes, MarkinchCurrent constituencyCreated2005Member of ParliamentPeter Grant (SNP)Created fromCentral Fife Glenrothes (/ɡlɛnˈrɒθɪs/) is a constituency in Scotland represented in the House of Commons of the UK Parliament sinc...

هذه المقالة عن المجموعة العرقية الأتراك وليس عن من يحملون جنسية الجمهورية التركية أتراكTürkler (بالتركية) التعداد الكليالتعداد 70~83 مليون نسمةمناطق الوجود المميزةالبلد القائمة ... تركياألمانياسورياالعراقبلغارياالولايات المتحدةفرنساالمملكة المتحدةهولنداالنمساأسترالي�...

Сельское поселение России (МО 2-го уровня)Новотитаровское сельское поселение Флаг[d] Герб 45°14′09″ с. ш. 38°58′16″ в. д.HGЯO Страна Россия Субъект РФ Краснодарский край Район Динской Включает 4 населённых пункта Адм. центр Новотитаровская Глава сельского пос�...

莫里斯·顾夫·德姆维尔法国总理任期1968年7月10日—1969年6月20日总统夏尔·戴高乐阿兰·波厄(英语:Alain Poher) (代理)前任乔治·蓬皮杜继任雅克·沙邦-戴尔马外交部长任期1958年6月1日—1968年5月30日总统勒内·科蒂夏尔·戴高乐总理米歇尔·德勃雷乔治·蓬皮杜前任勒内·普利文继任米歇尔·德勃雷 个人资料出生1907年1月24日兰斯逝世1999年12月24日(1999歲—12—24)(92歲)巴黎职业�...

Sporting event delegationBulgaria at the2008 Summer OlympicsIOC codeBULNOCBulgarian Olympic CommitteeWebsitewww.bgolympic.org (in Bulgarian and English)in BeijingCompetitors72 in 16 sportsFlag bearers Petar Stoychev (opening)Matey Kaziyski (closing)MedalsRanked 42nd Gold 1 Silver 1 Bronze 3 Total 5 Summer Olympics appearances (overview)18961900–1920192419281932193619481952195619601964196819721976198019841988199219962000200420082012201620202024 Bulgaria was represented by 72 athlet...

لمعانٍ أخرى، طالع ماركوس جونز (توضيح). هذه المقالة يتيمة إذ تصل إليها مقالات أخرى قليلة جدًا. فضلًا، ساعد بإضافة وصلة إليها في مقالات متعلقة بها. (يوليو 2019) ماركوس جونز (بالإنجليزية: Monty Jones) معلومات شخصية الميلاد 5 فبراير 1951 فريتاون تاريخ الوفاة 28 أبريل 2024 (73 ...
Play written by Samuel A. Taylor Sabrina FairFirst edition 1954Written bySamuel A. TaylorCharactersLinus Larrabee Jr.Sabrina FairchildDavid LarrabeeMaude Larrabee, Julia Ward McKinlock, Linus Larrabee Sr., Margaret, Gretchen, Mr. Fairchild, A Young Woman, A Young Man, Another Young Woman, Another Young Man, Paul D'ArgensonDate premieredNovember 11, 1953Place premieredNational TheatreNew York City, New YorkOriginal languageEnglishGenreRomantic ComedySettingThe North Shore of Long Island about ...

Colobothea hirtipes Klasifikasi ilmiah Kerajaan: Animalia Filum: Arthropoda Kelas: Insecta Ordo: Coleoptera Famili: Cerambycidae Genus: Colobothea Spesies: Colobothea hirtipes Colobothea hirtipes adalah spesies kumbang tanduk panjang yang tergolong famili Cerambycidae. Spesies ini juga merupakan bagian dari genus Colobothea, ordo Coleoptera, kelas Insecta, filum Arthropoda, dan kingdom Animalia. Larva kumbang ini biasanya mengebor ke dalam kayu dan dapat menyebabkan kerusakan pada batang kay...

Political party in Moldova National Alternative Movement Mișcarea Alternativa NaționalăAbbreviationMANLeaderIon CebanFounderIon CebanFounded22 December 2022 (2022-12-22)Registered17 January 2023 (2023-01-17)Split fromParty of Socialists of the Republic of MoldovaIdeologySocial democracyPro-EuropeanismPolitical positionCentre-leftParliament1 / 101District Presidents0 / 32Websitealternativa.euPolitics of MoldovaPolitical partiesElections The Nation...
