Dens evaginatus
| |||||||
Read other articles:

Party position in the Australian Senate Whips have managed business and maintained party discipline for Australia's federal political parties in the Senate since Federation. The term has origins in the British parliamentary system. Though the Remuneration Tribunal and parliamentary website refer to the senior Labor and Liberal whips as chief whips and their junior whips as deputy whips, the parties tend to refer to the senior whips as whips when announcing their officeholders to the Senate.&#...

Basilika Bunda BiaraBasilika Minor Bunda BiaraPortugis: Basilica de Nossa Senhora da Abadiacode: pt is deprecated Basilika Bunda BiaraLokasiUberabaNegara BrasilDenominasiGereja Katolik RomaArsitekturStatusBasilika minorStatus fungsionalAktif Basilika Bunda Biara (Portugis: Basilica de Nossa Senhora da Abadiacode: pt is deprecated ) adalah sebuah gereja basilika minor Katolik yang terletak di Uberaba, Brasil. Basilika ini ditetapkan statusnya pada tahun 2020 dan didedikasikan kepada Bunda...

American politician John Charles TarsneyMember of the U.S. House of Representativesfrom Missouri's 5th districtIn officeMarch 4, 1889 – February 27, 1896Preceded byWilliam WarnerSucceeded byRobert T. Van Horn Personal detailsBorn(1845-11-07)November 7, 1845Medina Township, Michigan, U.S.DiedSeptember 4, 1920(1920-09-04) (aged 74)Kansas City, Missouri, U.S.Resting placeMount St. Mary’s Cemetery, Kansas City, MissouriSpouseMary Behan (m. 1871-1917, her death)Relati...

العلاقات البنينية الطاجيكستانية بنين طاجيكستان بنين طاجيكستان تعديل مصدري - تعديل العلاقات البنينية الطاجيكستانية هي العلاقات الثنائية التي تجمع بين بنين وطاجيكستان.[1][2][3][4][5] مقارنة بين البلدين هذه مقارنة عامة ومرجعية للدولتين: وج�...

Cet article est une ébauche concernant une localité italienne et le Piémont. Vous pouvez partager vos connaissances en l’améliorant (comment ?) selon les recommandations des projets correspondants. Nichelino Armoiries Nom piémontais Ël Niclin Administration Pays Italie Région Piémont Ville métropolitaine Turin Code postal 10042 Code ISTAT 001164 Code cadastral F889 Préfixe tel. 011 Démographie Gentilé nichelinesi Population 46 244 hab. (1er janvier 20...

Davide Astori Astori con la nazionale italiana nel 2015 Nazionalità Italia Altezza 189 cm Peso 80 kg Calcio Ruolo Difensore CarrieraGiovanili 1995-1999 San Pellegrino1999-2001 Ponte San Pietro2001-2005 MilanSquadre di club1 2005-2006 Milan0 (0)2006-2007→ Pizzighettone25 (1)[1]2007-2008→ Cremonese31 (0)[2]2008-2014 Cagliari174 (3)2014-2015→ Roma24 (1)2015-2018 Fiorentina91 (3)Nazionale 2004-2005 Italia U-184 (0)2011-2017 ...

KylesaI Kylesa dal vivo nel 2011 Paese d'origine Stati Uniti(Savannah, GA) GenereSludge metal[1] Periodo di attività musicale2001 – in attività EtichettaPrank Records, At A Loss Recordings, Prosthetic Records, Season of Mist Album pubblicati9 Studio7 Live1 Raccolte1 Sito ufficiale Modifica dati su Wikidata · Manuale I Kylesa sono un gruppo sludge metal statunitense, formatosi nel 2001 a Savannah, Georgia. Il nome del gruppo deriva dall'espressione bud...

On finding a maximal set of solutions of a system of first-order homogeneous linear PDEs For other theorems named after Frobenius, see Frobenius theorem. The 1-form dz − y dx. on R3 maximally violates the assumption of Frobenius' theorem. These planes appear to twist along the y-axis. It is not integrable, as can be verified by drawing an infinitesimal square in the x-y plane, and follow the path along the one-forms. The path would not return to the same z-coordinate after one circuit. In m...

Judicial body in the United Kingdom Judicial Committee of the Privy CouncilArms as used by the Privy Council Office (United Kingdom) as of 2024[update][1]51°30′01.3″N 0°07′41.3″W / 51.500361°N 0.128139°W / 51.500361; -0.128139Established14 August 1833Jurisdiction List of countries Antigua and Barbuda The Bahamas Grenada Jamaica St. Kitts and Nevis St. Vincent and the Grenadines Tuvalu Cook Isla...

هذه المقالة يتيمة إذ تصل إليها مقالات أخرى قليلة جدًا. فضلًا، ساعد بإضافة وصلة إليها في مقالات متعلقة بها. (يونيو 2023) إسبانياEspaña (بالإسبانية) معلومات عامةبلد المنشأ المغرب التأسيس 1938 الاختفاء 1967 أول نشر 12 أكتوبر 1938آخر نشر 31 أكتوبر 1971القطع ورقيشخصيات هامةالمؤسس جريجوريو...

Dirty red color For other uses, see Burgundy (disambiguation). Wine red redirects here. For the RAL color, see Wine red (RAL). Burgundy Color coordinatesHex triplet#800020sRGBB (r, g, b)(128, 0, 32)HSV (h, s, v)(345°, 100%, 50%)CIELChuv (L, C, h)(26, 79, 7°)Source[1][2][3]ISCC–NBS descriptorPurplish red (pR)B: Normalized to [0–255] (byte) Burgundy is a dirty red.[4][5] European Union passports are usually burgundy in color...

Woodworking joint This article needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed.Find sources: Bridle joint – news · newspapers · books · scholar · JSTOR (February 2008) (Learn how and when to remove this message) Corner bridle joint T-bridle joint A bridle joint is a woodworking joint, similar to a mortise and tenon, in that a tenon is...

British supermarket chain This article is about the British supermarket. For other uses, see Morrison's (disambiguation) and Morrison (disambiguation). Wm Morrison Supermarkets LimitedLogo used since 2015Hilmore House in Bradford, Morrisons' head officeTrade nameMorrisonsCompany typePrivateIndustryRetailFounded1899; 125 years ago (1899)FounderWilliam MorrisonHeadquartersBradford, EnglandKey peopleRami Baitiéh (CEO)ProductsBooksClothingFloristFood and drinkHomewareMagazinesP...

يفتقر محتوى هذه المقالة إلى الاستشهاد بمصادر. فضلاً، ساهم في تطوير هذه المقالة من خلال إضافة مصادر موثوق بها. أي معلومات غير موثقة يمكن التشكيك بها وإزالتها. (ديسمبر 2018) 50° خط عرض 50 جنوب خريطة لجميع الإحداثيات من جوجل خريطة لجميع الإحداثيات من بينغ تصدير جميع الإحداثيات من ك...

Come leggere il tassoboxAcero opaloAcer opalus subsp. obtusatumClassificazione APG IVDominioEukaryota RegnoPlantae (clade)Angiosperme (clade)Mesangiosperme (clade)Eudicotiledoni (clade)Eudicotiledoni centrali (clade)Superrosidi (clade)Rosidi (clade)Eurosidi (clade)Malvidi OrdineSapindales FamigliaSapindaceae SottofamigliaHippocastanoideae TribùAcereae GenereAcer SpecieA. opalus Classificazione CronquistDominioEukaryota RegnoPlantae DivisioneMagnoliophyta ClasseMagnoliopsida OrdineSapindales ...

Myles BurnyeatCBE FBALahirMyles Fredric Burnyeat1 Januari 1939London, Inggris[1]Meninggal20 September 2019 (usia 80)Latar belakang akademisAlma materKing's College, CambridgeUniversity College, LondonPenasihat akademikBernard WilliamsKarya akademisDisiplin ilmuFilsafatCabang disiplin ilmuFilsafat kunoLembagaRobinson College, CambridgeAll Souls College, OxfordMahasiswa ternamaAngie Hobbs Penghargaan Commander of the Order of the British Empire (en) Fellow of the British Academy My...
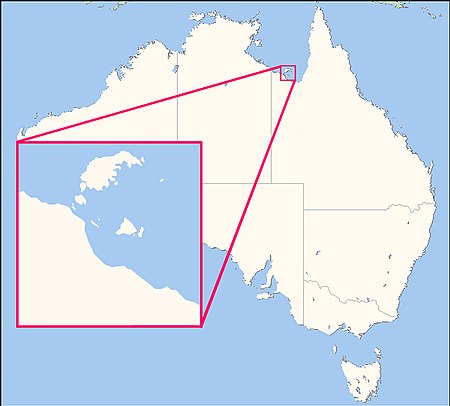
Australian Aboriginal language KayardildRegionSouth Wellesley Islands, north west Queensland, AustraliaEthnicityKaiadilt, YanggalNative speakers8 (2016 census)[1]Language familyMacro-Pama–Nyungan? TangkicKayardildDialects Kayardild Yangkaal[2] Language codesISO 639-3Either:gyd – Kayardildnny – Yangkaal/Nyangga (two different languages)Glottologkaya1318AIATSIS[3]G35 Kayardild, G37 YangkaalELPKayardild Yangkaal[4]Kaya...

French diplomat (1754–1838), Prime Minister of France in 1815 His Serene HighnessCharles-Maurice de Talleyrand-PérigordPrince of TalleyrandPortrait by Pierre-Paul Prud'hon (1817)Ambassador of France to the United KingdomIn office6 September 1830 – 13 November 1834Appointed byLouis Philippe IPreceded byPierre de Montmercy-LavalSucceeded byHorace Sébastiani de La PortaPrime Minister of FranceIn office9 July 1815 – 26 September 1815MonarchLouis XVIIIPreceded byOffice es...

Cet article est une ébauche concernant une localité italienne et la Lombardie. Vous pouvez partager vos connaissances en l’améliorant (comment ?) selon les recommandations des projets correspondants. Castello Cabiaglio Armoiries Drapeau Noms Nom latin (origine) cavea ou capulum Administration Pays Italie Région Lombardie Province Varèse Code postal 21030 Code ISTAT 012043 Code cadastral B312 Préfixe tel. 0332 Démographie Gentilé cabiagliesi Population 548 hab....

English landowner and politician Sir Wilfrid Lawson, 1st Baronet, of Isel Hall, Cumberland (c. 1610–1688) was an English landowner and politician who sat in the House of Commons from 1660 to 1679. Isel Hall, Cumbria in 1892 Life Lawson was born in 1610, the son of William Lawson, and his wife Judith Bewley, daughter of William Bewley of Hesket. His great uncle was Sir Wilfred Lawson who acquired the family estate of Isel in Elizabethan times and served as MP for Cumberland. Lawson matr...