Triploid syndrome
| |||||||||||||
Read other articles:

Komisi Pengawas Nasional Republik Rakyat Tiongkok中华人民共和国国家监察委员会Zhōnghuá Rénmín Gònghéguó Guójiā Jiānchá WěiyuánhuìKantor pusat Komisi Pengawas Nasional diJalan Ping'anli Barat 41, Distrik Xicheng, BeijingNamaKomisi Pengawas NasionalIkhtisarDibentuk23 Maret 2018Struktur yurisdiksiLembaga nasionalTiongkokWilayah hukumTiongkokMarkas besarBeijing, TiongkokPejabat pemerintahYang Xiaodu, Direktur Komisi Pengawas NasionalSitus webCCDI & NSC official webs...

4TEN4TEN di Hello, Mr K! Concert, pada April 2016Informasi latar belakangNama lainPOTENAsalSeoul, Korea SelatanGenreK-popDance-popHip hopTahun aktif2014 (2014)–sekarangLabelJungle EntertainmentAnggota Hyeji Hyejin Heeo Jisoo Mantan anggota TEM Eujin Hajeong Yun 4Ten (Hangul:포텐, sebelumnya POTEN), umumnya ditulis sebagai 4TEN, adalah grup vokal wanita asal Korea Selatan yang dibentuk oleh Jungle Entertainment pada tahun 2014.[1] Grup ini pada saat ini terdiri dari empat angg...

إيزابيلا من البرتغال ملكة قشتالة وليون القرينة فترة الحكم22 يوليو 1447 - 20 يوليو 1454 معلومات شخصية الميلاد 1428مملكة البرتغال الوفاة 15 أغسطس 1496أريفالو مواطنة مملكة البرتغال الديانة الكنيسة الرومانية الكاثوليكية الزوج خوان الثاني ملك قشتالة (22 يوليو 1447–22 يونيو 1454) ال�...

الدوري المنغولي لكرة القدم 2001 تفاصيل الموسم الدوري المنغولي لكرة القدم البلد منغوليا الدوري المنغولي لكرة القدم 2000 الدوري المنغولي لكرة القدم 2002 تعديل مصدري - تعديل الدوري المنغولي لكرة القدم 2001 هو موسم من الدوري المنغولي لكرة القدم. فاز فيه Khangarid FC [ال�...

Este artículo o sección tiene referencias, pero necesita más para complementar su verificabilidad. Busca fuentes: «Comercio electrónico» – noticias · libros · académico · imágenesEste aviso fue puesto el 10 de octubre de 2020. Explicación gráfica de como funciona.El comercio electrónico[1] está constituido por transacciones comerciales que se realizan a través de Internet, mientras que el negocio electrónico utiliza las tecnologías de informació...

هذه مقالة غير مراجعة. ينبغي أن يزال هذا القالب بعد أن يراجعها محرر؛ إذا لزم الأمر فيجب أن توسم المقالة بقوالب الصيانة المناسبة. يمكن أيضاً تقديم طلب لمراجعة المقالة في الصفحة المخصصة لذلك. (أكتوبر 2021) قائمة المهام إلى الكواكب الصغيرة هي قائمة بعثات الرحلات الفضائية إلى الكو...

Chemical reaction that gives browned food flavor The crusts of most breads, such as this brioche, are golden-brown mostly as a result of the Maillard reaction. The Maillard reaction (/maɪˈjɑːr/ my-YAR; French: [majaʁ]) is a chemical reaction between amino acids and reducing sugars to create melanoidins, the compounds which give browned food its distinctive flavor. Seared steaks, fried dumplings, cookies and other kinds of biscuits, breads, toasted marshmallows, and many other foo...

This article needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed.Find sources: 1st Cherokee Mounted Rifles – news · newspapers · books · scholar · JSTOR (September 2015) (Learn how and when to remove this message) Regiment of the Confederate States Army 1st Cherokee Mounted RiflesNational Color of the1st Cherokee Mounted RiflesActive1861�...

Angelo InfantiAngelo Infanti dalam Talcum Powder, 1982Lahir(1939-02-16)16 Februari 1939Zagarolo, ItaliaMeninggal12 Oktober 2010(2010-10-12) (umur 71)Tivoli, ItaliaPekerjaanPemeranTahun aktif1961–2010 Angelo Infanti (pelafalan dalam bahasa Italia: [ˈandʒelo infanˈti]; 16 Februari 1939 – 12 Oktober 2010) adalah seorang pemeran film asal Italia. Ia tampil dalam lebih dari 90 film antara 1961 dan 2010.[1] Referensi ^ Angelo Infanti. The New York Tim...

في الهندسة النووية, مهدئ النيوترون هو عبارة عن وسيط يقوم بتقليص سرعة النيوترونات السريعة, ويذبل يتم تحويلها إلى نيوترونات حرارية قادرة على الحفاظ على التفاعل النووي المتسلسل لليورانيوم-235. هناك العديد من المواد الشائعة تُستعمل كمهدئات ومن ضمنها الماء (الخفيف) العادي (تُست�...
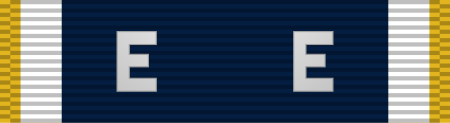
US Navy award This article needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed.Find sources: Navy E Ribbon – news · newspapers · books · scholar · JSTOR (May 2008) (Learn how and when to remove this message) AwardNavy E RibbonNavy E Ribbon, from top to bottom. first through fourth and final awards.Awarded forBattle efficiency (cited ships...

Politics of the Turks and Caicos Islands Constitution Monarchy Sovereign Charles III Governor Dileeni Daniel-Selvaratnam Deputy Governor of the Turks and Caicos Islands Anya Williams Executive Premier Washington Misick Cabinet Legislative House of Assembly Speaker: Gordon Burton Elections Recent elections General: 2007201220162021 Political parties Progressive NationalParty (PNP) People's DemocraticMovement (PDM) Administrative divisions Citizenship Belonger status British Overseas Territorie...

Coronación de Victoria del Reino Unido Óleo de la coronación de la reina Victoria del Reino UnidoLocalizaciónPaís Reino UnidoLugar Abadía de WestminsterDatos generalesTipo Coronación del monarca británicoParticipantes Victoria del Reino Unido Oficiales de Estado del Reino Unido Obispos y Arzobispos de la Iglesia de InglaterraOrden de la Jarretera Nobles del Reino UnidoHistóricoFecha 28 de junio de 1838[editar datos en Wikidata] La coronación de la reina Victoria del Reino ...

A rapid transit line of the Doha Metro Red LineOverviewOther name(s)Coastal LineNative nameالخط الأحمرStatusOperatingOwner Government of QatarLocaleDoha, QatarTerminiLusail Hamad International Airport T1 Al Wakra Stations18ServiceTypeRapid transitSystemDoha MetroServices Lusail ↔ Hamad International Airport T1 Lusail ↔ Al Wakra Operator(s) Qatar RailRolling stockMitsubishi Corporation and Kinki SharyoHistoryOpened8 May 2019 (2019-05-08)TechnicalLine length40 ...

1976 Turkish filmHababam Sınıfı Sınıfta KaldıDirected byErtem EğilmezWritten bySadik SendilRıfat Ilgaz (novel)Produced byErtem EğilmezStarringKemal SunalAdile NaşitHalit AkçatepeTarık AkanCinematographyKriton IlyadisMusic byMelih KibarProductioncompanyArzu FilmRelease date 1 January 1976 (1976-01-01) Running time91 mins.CountryTurkeyLanguageTurkish Hababam Sınıfı Sınıfta Kaldı (The Chaos Class Failed The Class) is a 1975 Turkish comedy film, directed by Ertem ...

Ular-cokelat Australia Pseudonaja TaksonomiKerajaanAnimaliaFilumChordataKelasReptiliaOrdoSquamataFamiliElapidaeGenusPseudonaja Günther, 1858 Ular-cokelat Australia atau dalam bahasa Inggris disebut brownsnakes adalah sebutan umum untuk jenis-jenis ular berbisa Elapidae yang diklasifikasikan sebagai genus Pseudonaja (yang bermakna kobra palsu).[1] Ular-ular ini tersebar luas di Australia. Salah satu spesies, yaitu ular-cokelat timur (P. textilis), juga tersebar di sebagian Pulau Papua...

In azzurro scuro è l'estensione limitata dell'Occidente (il Nord America, l'Europa cattolica e protestante, l'Australia e la Nuova Zelanda), come definito da Samuel P. Huntington nel suo libro Lo scontro delle civiltà (1996), ed, in azzurro chiaro, l'Europa ortodossa e l'America Latina. Per Huntington, l'Europa ortodossa è la parte orientale dell'Occidente, mentre l'America Latina faceva parte dell'Occidente o di una civiltà discendente che era gemellata con esso[1]. Con civiltà ...

Bagian dari Elevated Walkway, Forest Walk, Telok Blangah Hill Park Telok Blangah Hill Park adalah taman yang terletak di Telok Blangah Green, pinggir Henderson Road, di Bukit Merah, Singapura. Sejarah Sejak awal abad ke-19, taman ini menjadi tempat bertemunya komunitas pedagang. Salah satu bukti kekayaan para pedagang ini adalah Alkaff Mansion, bungalow kolonial yang dibangun oleh seorang pedagang Arab dan pernah dijadikan gedung pesta besar untuk kalangan elit.[1] Lihat pula Daftar t...

Jakub VeselýNazionalità Rep. Ceca Altezza206 cm Pallavolo RuoloCentrale Squadra Saint-Nazaire CarrieraGiovanili 2002-2003 Olomouc Squadre di club 2003-2008 Dukla Liberec2008-2011 Arago de Sète2011-2012 Piemonte2012-2013 Modena2013-2014 AZS Częstochowa2014-2015 Saint-Nazaire2015-2016 Benátky nad Jizerou2016- Dukla Liberec Nazionale 2007- Rep. Ceca Statistiche aggiornate al 7 agosto 2013 Modifica dati su Wikidata · Manuale Ja...

هذه المقالة يتيمة إذ تصل إليها مقالات أخرى قليلة جدًا. فضلًا، ساعد بإضافة وصلة إليها في مقالات متعلقة بها. (يناير 2021) فريدريكا غوزمان معلومات شخصية الميلاد 23 مايو 1981 (43 سنة) كاراكاس مواطنة فنزويلا الحياة العملية المهنة عارضة، ومتسابقة ملكة الجمال تعديل مصدر�...
