Berlin Patient
| |||||||||
Read other articles:

SMP Negeri 3 JemberSekolah Menengah Pertama Negeri 3 JemberInformasiDidirikan5 Juli 1977JenisNegeriAkreditasiANomor Pokok Sekolah Nasional20523891Kepala SekolahHeru Wahyudi, S.Pd., M.Pd.Jumlah kelas25 KelasRentang kelasVII, VIII, IXKurikulumKurikulum Merdeka (Kelas 7) Kurikulum 2013 (Kelas 8, 9)Jumlah siswa807 siswaAlamatLokasiJl. Jawa No. 8, Tegal Boto Lor, Sumbersari, Jember, Jawa Timur, Tel./Faks.0331-334335Koordinat--8.168876,113.712344Situs webwww.smpn3jember.sch.idLa...

لوتراكي Λουτράκι Loutraki (باليونانية: Λουτράκι) تقسيم إداري البلد اليونان[1] المنطقة الإدارية البيلوبونيز كورينثيا خصائص جغرافية إحداثيات 37°58′30″N 22°58′36″E / 37.975°N 22.976666666667°E / 37.975; 22.976666666667 الأرض 196.870 كم² الارتفاع 82 متر السكان التعداد السكاني 15...

العلاقات الإريترية السيشلية إريتريا سيشل إريتريا سيشل تعديل مصدري - تعديل العلاقات الإريترية السيشلية هي العلاقات الثنائية التي تجمع بين إريتريا وسيشل.[1][2][3][4][5] مقارنة بين البلدين هذه مقارنة عامة ومرجعية للدولتين: وجه المقارنة إريت�...

This article is about the restaurant in New York City. For other uses, see Odeon. Restaurant in New York, United StatesThe OdeonThe restaurant's exterior in 2009Restaurant informationStreet address145 West BroadwayCityNew York CityStateNew YorkCountryUnited StatesCoordinates40°43′01″N 74°00′28″W / 40.716967°N 74.007841°W / 40.716967; -74.007841 The Odeon is a restaurant in New York City.[1] The restaurant opened in 1980, in space previously occupie...

Синелобый амазон Научная классификация Домен:ЭукариотыЦарство:ЖивотныеПодцарство:ЭуметазоиБез ранга:Двусторонне-симметричныеБез ранга:ВторичноротыеТип:ХордовыеПодтип:ПозвоночныеИнфратип:ЧелюстноротыеНадкласс:ЧетвероногиеКлада:АмниотыКлада:ЗавропсидыКласс:Пт�...

Japanese cargo airline Nippon Cargo Airlines日本貨物航空 IATA ICAO Callsign KZ NCA NIPPON CARGO FoundedSeptember 21, 1978; 45 years ago (1978-09-21)HubsNaha[1]Osaka–KansaiTokyo–NaritaFocus citiesAnchorageHong KongFleet size8Destinations20Parent companyNippon YusenHeadquartersNarita International AirportNarita, Chiba, JapanKey peopleTetsufumi Otsuki (President & CEO)Websitewww.nca.aero Nippon Cargo Airlines Company, Limited (日本貨物航空株式会�...

本表是動態列表,或許永遠不會完結。歡迎您參考可靠來源來查漏補缺。 潛伏於中華民國國軍中的中共間諜列表收錄根據公開資料來源,曾潛伏於中華民國國軍、被中國共產黨聲稱或承認,或者遭中華民國政府調查審判,為中華人民共和國和中國人民解放軍進行間諜行為的人物。以下列表以現今可查知時間為準,正確的間諜活動或洩漏機密時間可能早於或晚於以下所歸�...

Australian chemist (1910–1962) Frank DwyerBorn(1910-12-03)3 December 1910Raymond Terrace, New South WalesDied22 June 1962(1962-06-22) (aged 51)CanberraAlma materUniversity of SydneyOccupationProfessor of ChemistryEmployer(s)Sydney Technical College (until 1946), University of Sydney (1946-1957), Pennsylvania State University (1956-1962), John Curtin School of Medical Research (1959-1962)Scientific careerDoctoral students Brice Bosnich Alan Sargeson[1] Francis Patrick John ...

Ballast carried to counteract buoyancy Weight belt redirects here. For the belt used to support the torso during strength training, see Weight lifting belt. Conventional scuba weight-belt with quick-release buckleOther namesDive weightsWeight-beltIntegrated weightsTrim weightsUsesBuoyancy correction and trim adjustment of underwater diversRelated itemsBuoyancy compensation device A bag weight belt and a traditional weight belt A diving weighting system is ballast weight added to a diver or di...

American assessor, auditor, Justice of the Peace, teacher and Revolutionary War veteran Wentworth CheswellBorn(1746-04-11)11 April 1746Newmarket, New HampshireDied8 March 1817(1817-03-08) (aged 70)Burial placeNewmarket, New HampshireNationalityAmericanOther namesWentworth CheswillEducationGovernor Dummer AcademyOccupation(s)Teacher, soldier, town officialKnown forfirst black man elected to public office in the United States, and first black judge in the U.S.SpouseMary DavisChil...
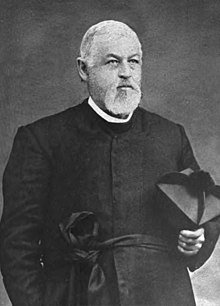
Hannibal GoodwinLahir(1822-04-21)21 April 1822Taughannock, New YorkMeninggal31 Desember 1900(1900-12-31) (umur 78) Hannibal Williston Goodwin (21 April 1822 – 31 Desember 1900), adalah seorang pendeta episkopal di Rumah Doa Gereja Episkopal dan Pastoran di Newark, New Jersey, pembuat gulungan tembus cahaya keluaran film dari dasar film nitroselulosa, yang digunakan pada Kinetoskop milik Thomas Edison, mesin awal untuk melihat sebuah animasi.[1] Referensi ^ Greg Hatala (17 Dece...

New Park Theatre redirects here. For the earlier theater of the same name, see Abbey's Park Theatre. Former theatre in Manhattan, New York Herald Square TheatreHerald Square Theatre in 1907Former names(New) Park Theatre (1883–1894)Address1331 BroadwayNew York CityUnited StatesTypeBroadwayCapacity1150ConstructionOpened1883Closed1914 (1914)Demolished1915Years active1883–1914ArchitectRose & Stone The Herald Square Theatre was a Broadway theatre in Manhattan, New York City, built in ...

此條目没有列出任何参考或来源。 (2016年7月23日)維基百科所有的內容都應該可供查證。请协助補充可靠来源以改善这篇条目。无法查证的內容可能會因為異議提出而被移除。 安装在深空一号上的NASA的2.3 kW NSTAR离子推力器正在喷气推进实验室里试验 蘇聯製SPT离子推力器系列 離子推力器(Ion thruster, ion drive),又稱离子推进器、離子發動機,其原理是先將氣體電離,然後用電�...

维克托·丘卡林出生1921年11月9日 Khreshchatytske 逝世1984年8月25日 (62歲)利沃夫 安葬于利查基夫公墓 就讀學校Lviv State University of Physical Culture 職業竞技体操运动员、體操運動員 僱主Lviv State University of Physical Culture 政党苏联共产党 维克托·伊万诺维奇·丘卡林(俄語:Виктор Иванович Чукарин,烏克蘭語:Віктор Іванович Чука...

New York City government agency Department of Environmental ProtectionDepartment overviewJurisdictionNew York CityHeadquarters59-17 Junction BoulevardElmhurst, QueensEmployees6,210 (2020[update])[1]Department executivesRohit T. Aggarwala, Commissioner of Environmental ProtectionVincent Sapienza, Chief Operating OfficerKey documentNew York City CharterWebsitewww.nyc.gov/dep Tallman Island plant Rockaway plant Sludge boat passing under the Brooklyn Bridge on the East River The N...

Molten salt reactor prototype For other uses of the acronym, see TMSR (disambiguation). TMSR-LF1TMSR project logoGenerationIVReactor conceptMSRStatusPending[1]LocationChina[note] Maps class=notpageimage| TMSR-LF1 (trefoil) in Gansu province (red). Shanghai campus also indicated. TMSR-LF1 (trefoil) within Minqin county (orange) is roughly 120 km (75 miles) north of the city of Wuwei (star)[2] Coordinates38°57′37″N 102°36′44″E / 38.9602°N 102.6122°E&#...

Church in Provence-Alpes-Côte d'Azur, FranceÉglise Saint-Vincent-de-PaulLocation8 cours Franklin RooseveltMarseille 13001Bouches-du-Rhône, Provence-Alpes-Côte d'AzurCountryFranceDenominationRoman Catholic ChurchHistoryDedicated1886ArchitectureArchitect(s)François ReybaudArchitectural typechurchStyleGothicAdministrationDioceseRoman Catholic Archdiocese of MarseilleClergyPriest(s)Philippe Rochas The Église Saint-Vincent-de-Paul (Les Réformés) is a Roman Catholic church in Marseille, Fra...

This article is about the geographical plain between North Macedonia and Greece. For the political unit in North Macedonia, see Pelagonia Statistical Region. Not to be confused with Palagonia. Location of Pelagonia Pelagonia seen from Baba Mountain, Bitola. Pelagonia (Macedonian: Пелагонија, romanized: Pelagonija; Greek: Πελαγονία, romanized: Pelagonía) is a geographical region of Macedonia named after the ancient kingdom. Ancient Pelagonia roughly corresponded t...

Geological structure and composition of Venus This article needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed.Find sources: Geology of Venus – news · newspapers · books · scholar · JSTOR (February 2020) (Learn how and when to remove this message) Radar global map of the surface of Venus The hemispheric view of Venus, as revealed by more ...

Pragmatic methodology Part of a series onEvidence-based practices Assessment Design Management Research Scheduling Dentistry Medical ethics Medicine Nursing Pharmacy Toxicology Conservation Education Legislation Library and information practice Policy Policing Prosecution vte Evidence-based practice is the idea that occupational practices ought to be based on scientific evidence. The movement towards evidence-based practices attempts to encourage and, in some instances, require professionals ...
