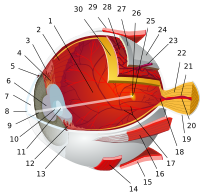
Ocular immune system
|
Read other articles:

Daftar tokoh Jambi ini memuat nama tokoh-tokoh yang lahir atau keturunan dan berperan di Provinsi Jambi. Khusus mengenai tokoh-tokoh dari Kota Jambi, dan Kota Sungai Penuh bisa dilihat di Daftar tokoh Kota Jambi, dan Daftar tokoh Kota Sungai Penuh. Perangkat pemantau ini bisa digunakan untuk melihat perubahan terbaru dari artikel-artikel yang terkait dengan halaman ini. Jika pembaca melihat artikel tokoh di Wikipedia bahasa Indonesia yang semestinya masuk ke dalam daftar ini, silakan sunting ...

لمعانٍ أخرى، طالع نيويورك (توضيح). نيويورك علم شعار الشعار:(باللاتينية: Excelsior) (1778–) الإحداثيات 43°N 75°W / 43°N 75°W / 43; -75 [1] تاريخ التأسيس 26 يوليو 1788 سبب التسمية دوق يورك تقسيم إداري البلد الولايات المتحدة[2][3] الت�...

Urban contemporary radio station in Chicago WGCI-FMChicago, IllinoisBroadcast areaChicago metropolitan areaNorthwest IndianaFrequency107.5 MHz (HD Radio)Branding107.5 WGCIProgrammingLanguage(s)EnglishFormatUrban contemporaryAffiliationsPremiere NetworksOwnershipOwneriHeartMedia(iHM Licenses, LLC)Sister stationsWCHI-FMWGRBWKSC-FMWLIT-FMWVAZWVONHistoryFirst air dateDecember 4, 1958(65 years ago) (1958-12-04)[1]Former call signsWFMQ (1958–65)[2]WNUS-FM (1965–75)[...

Ini adalah nama Korea; marganya adalah Kim. Kim Yeong-cheolLahir25 Februari 1953 (umur 71)Daegu, Provinsi Gyeongsang Utara, Korea SelatanNama lainKim Young-chulPekerjaanAktorTahun aktif1986-sekarangSuami/istriLee Moon-hee (aktris)Anak2 putraNama KoreaHangul김영철 Hanja金永哲 Alih AksaraGim Yeong-cheolMcCune–ReischauerKim Yŏng-ch‘ŏl Kim Yeong-cheol (lahir 25 Februari 1953) adalah aktor asal Korea Selatan. Salah satu dari penampilan awalnya adalah di White Smile (1981...
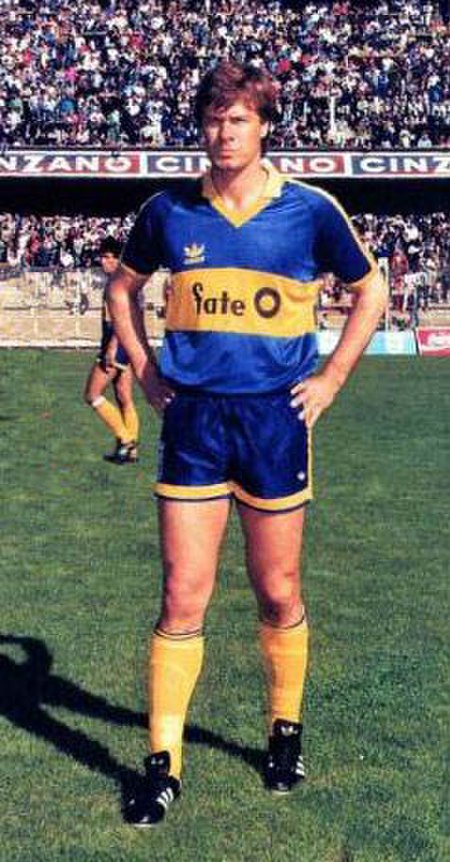
Argentine footballer Claudio Marangoni Marangoni while playing for Boca Juniors, 1988Personal informationFull name Claudio Oscar MarangoniDate of birth (1954-11-17) 17 November 1954 (age 69)Place of birth Rosario, ArgentinaHeight 1.86 m (6 ft 1 in)Position(s) MidfielderSenior career*Years Team Apps (Gls)1974–1976 Chacarita Juniors 62 (7)1976–1979 San Lorenzo 135 (25)1979–1980 Sunderland 20 (3)1981 Huracán 58 (11)1982–1988 Independiente 237 (25)1988–1990 Boca Jun...

Genus of plants Not to be confused with Liriodendron tulipifera (tulip poplar). For other uses, see Populus (disambiguation). PopulusTemporal range: 58–0 Ma PreꞒ Ꞓ O S D C P T J K Pg N Leaf of Populus tremula Scientific classification Kingdom: Plantae Clade: Tracheophytes Clade: Angiosperms Clade: Eudicots Clade: Rosids Order: Malpighiales Family: Salicaceae Subfamily: Salicoideae Tribe: Saliceae Genus: PopulusL. Type species Populus tremulaL. Sections and species See text Populus ...

Former theatre in Manhattan, New York Comedy Theatre Collier's Comedy Theatre (1910–13) Mercury Theatre (1937–40) Artef Theatre (1940–42) Address110 West 41st StreetNew York CityUnited StatesCoordinates40°45′16″N 73°59′07″W / 40.7543717°N 73.9853195°W / 40.7543717; -73.9853195OwnerThe Shubert OrganizationTypeBroadwayCapacity687ConstructionOpenedSeptember 6, 1909Demolished1942Years active1909–1942ArchitectD. G. Malcolm The Comedy Theatre was a Broadw...

1986 Indian filmKarnaSuperhit Karna movie posterDirected byH. R. BhargavaWritten byChi. Udaya ShankarScreenplay byH. R. BhargavaProduced byB. Anuradha SinghR. Dushyanth SinghR. Amritha SinghStarringVishnuvardhanSumalathaSumithraK. S. AshwathGangadharCinematographyD. V. RajaramEdited byV. P. KrishnaMusic byM. Ranga RaoProductioncompaniesAmrutha ArtsRohini PicturesDistributed byAmrutha ArtsRohini PicturesRelease date 10 January 1986 (1986-01-10) Running time148 minCountryIndiaLa...

Artikel ini sebatang kara, artinya tidak ada artikel lain yang memiliki pranala balik ke halaman ini.Bantulah menambah pranala ke artikel ini dari artikel yang berhubungan atau coba peralatan pencari pranala.Tag ini diberikan pada Oktober 2022. JallikattuJallikattuNama lainEru thazhuvuthal, Manju virattuPertama dimainkan400-100 BC[1]KarakteristikGender campurantidakKategoriolahraga tradisionalTempat bertandingTanah terbukaKeberadaanNegara atau wilayahTamil Nadu, IndiaOlimpiadetid...
Artikel ini perlu diterjemahkan dari bahasa Inggris ke bahasa Indonesia. Artikel ini ditulis atau diterjemahkan secara buruk dari Wikipedia bahasa Inggris. Jika halaman ini ditujukan untuk komunitas bahasa Inggris, halaman itu harus dikontribusikan ke Wikipedia bahasa Inggris. Lihat daftar bahasa Wikipedia. Artikel yang tidak diterjemahkan dapat dihapus secara cepat sesuai kriteria A2. Jika Anda ingin memeriksa artikel ini, Anda boleh menggunakan mesin penerjemah. Namun ingat, mohon tidak men...

British magazine of comics news and criticism Not to be confused with Speakeasy Comics. SpeakeasyThe cover of Speakeasy #65 (August 1986). Artwork by Brian Bolland.EditorRichard Ashford (1979–1986)Cefn Ridout (1986)Nigel Curson (1989–1990)Stuart Green (1990–1991)Categoriescomics, criticism, history, interviewsFrequencymonthlyPublisherRichard Ashford (1979–1986)Acme Press (1986–1989)John Brown Publishing (1989–1991)First issueAug. 1979Final issueNumberMay 1991120CountryUnited Kingd...

Hindu goddess of shadow For other uses, see Chhaya (disambiguation). ChhayaGoddess of ShadowsSurya with consorts Sanjna and ChhayaDevanagariछायाSanskrit transliterationChhāyāAffiliationDevi, shadow of SaranyuAbodeSuryalokaMantraOm Chhayave NamahPersonal informationConsortSuryaChildrenSavarni Manu, Shani, Tapati Chhaya or Chaya (Sanskrit: छाया, romanized: Chāyā, lit. 'shadow' or 'shade') is the Hindu personification and goddess of shadow, also called Sand...

Negatively charged polyatomic ion containing oxygenAn oxyanion, or oxoanion, is an ion with the generic formula AxOz−y (where A represents a chemical element and O represents an oxygen atom). Oxyanions are formed by a large majority of the chemical elements.[1] The formulae of simple oxyanions are determined by the octet rule. The corresponding oxyacid of an oxyanion is the compound HzAxOy. The structures of condensed oxyanions can be rationalized in terms of AOn polyhedral units wi...

American nonprofit organization Not to be confused with Jimmy Carter Library and Museum. The Carter CenterFoundedApril 6, 1982; 42 years ago (1982-04-06)[1]FounderJimmy CarterRosalynn Carter[1]TypeNot-for-profit, non-governmental organization(IRS exemption status): 501(c)(3)[1]Tax ID no. 58-1454716FocusHuman rights, Conflict resolution, Election monitoring, Public health, Eradication of infectious diseases, Mental healthLocationOne Copenhill453 Freedo...

Aslacton WindmillThe derelict mill in 2007OriginMill nameAslacton MillMill locationTM 1575 9037Coordinates52°28′07″N 1°10′29″E / 52.46861°N 1.17472°E / 52.46861; 1.17472Operator(s)PrivateYear built1834InformationPurposeCorn millTypeTower millStoreysFour storeysNo. of sailsFour sailsType of sailsDouble Patent sailsWindingFantailFantail bladesSix bladesAuxiliary powerSteam engine, later replaced by an oil engineNo. of pairs of millstonesTwo pairs Aslacton Mi...

هذه المقالة بحاجة لصندوق معلومات. فضلًا ساعد في تحسين هذه المقالة بإضافة صندوق معلومات مخصص إليها. لمعانٍ أخرى، طالع تلاش (توضيح). هذه المقالة يتيمة إذ تصل إليها مقالات أخرى قليلة جدًا. فضلًا، ساعد بإضافة وصلة إليها في مقالات متعلقة بها. (نوفمبر 2019) تلاش (منظومة صواريخ ...

For the hospital in Scotland, see Dunbar Hospital, Thurso. Hospital in Michigan, United StatesDunbar HospitalAllied Medical SocietyGeographyLocationMichigan, United StatesOrganizationFundingNon-profit hospitalTypeGeneralServicesBeds27HistoryFormer name(s)Parkside Hospital after 1928Opened1918Closed1962LinksListsHospitals in MichiganDunbar HospitalU.S. National Register of Historic PlacesMichigan State Historic Site Location580 Frederick StreetDetroit, MichiganCoordinates42°21′42″N 83°3�...

新市场广场 新市场广场(波兰语:plac Nowy Targ;德语:Neumarkt)是弗罗茨瓦夫的一个广场。它是老城三大历史广场之一,另外两个是盐市广场和中央集市广场。 历史 新市场广场是该市最古老的广场之一。它是日耳曼人在布雷斯劳建立的第一个定居点,1214年第一次见于记载。15世纪,广场南侧建起聖伯爾納鐸修道院。1732年,广场中央放置巴洛克风格的海神喷泉(Neptunbrunnen)�...

British economist SirAlan WaltersBorn(1926-06-17)17 June 1926Leicester, EnglandDied3 January 2009(2009-01-03) (aged 82)NationalityBritishSpouse Margaret Patricia Wilson (m. 1975)Academic careerFieldEconomicsInstitutionUniversity of BirminghamLondon School of EconomicsWorld BankJohns Hopkins UniversityAmerican Enterprise InstituteSchool ortraditionMonetarismAlma materUniversity College, LeicesterNuffield College, OxfordInfluencesErnest Cass...

For other people named Stefán Stefánsson, see Stefán Stefánsson (disambiguation). This is an Icelandic name. The last name is patronymic, not a family name; this person is referred to by the given name Stefán Jóhann. Stefán Stefánsson14th Prime Minister of IcelandIn office4 February 1947 – 6 December 1949PresidentSveinn BjörnssonPreceded byÓlafur ThorsSucceeded byÓlafur ThorsMinister of Foreign AffairsIn office18 November 1941 – 17 January 1942Prime MinisterHe...