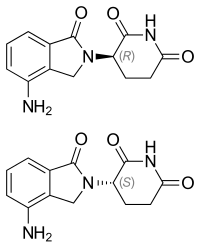
Lenalidomide
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Read other articles:

Artikel ini sebatang kara, artinya tidak ada artikel lain yang memiliki pranala balik ke halaman ini.Bantulah menambah pranala ke artikel ini dari artikel yang berhubungan atau coba peralatan pencari pranala.Tag ini diberikan pada Oktober 2022. Artikel ini tidak memiliki referensi atau sumber tepercaya sehingga isinya tidak bisa dipastikan. Tolong bantu perbaiki artikel ini dengan menambahkan referensi yang layak. Tulisan tanpa sumber dapat dipertanyakan dan dihapus sewaktu-waktu.Cari sumber:...

Hercules: The Legendary Journeys is an American television series based on the tales of the classical Greek hero, produced from January 16, 1995, to November 22, 1999. It had two spin-off series: Xena: Warrior Princess, which ran from 1995 to 2001, and the prequel Young Hercules, which ran in 1998 and 1999. This list includes significant characters from all three series. Main characters Main characters: (left to right) Gabrielle, Xena, Hercules and Iolaus Hercules (portrayed by Kevin Sorbo a...

Pour les articles homonymes, voir Pellicer. José PellicerBiographieNaissance 27 avril 1912ValenceDécès 8 juin 1942 (à 30 ans)Nationalité espagnoleActivités Anarcho-syndicaliste, mécanicien, homme politique, syndicaliste, anarchiste, anarchist militiamanAutres informationsIdéologie AnarchismeMembre de Confédération nationale du travailLos SolidariosMilices confédéralesColonne de fer (en)modifier - modifier le code - modifier Wikidata José Pellicer Gandía, né le 27 avril 19...

Teatro NazionaleUbicazioneStato Italia LocalitàMilano IndirizzoVia Giordano Rota, 1 - ex Piazza Piemonte, 12 - 20149 Dati tecniciFossapresente Capienza1 500 posti RealizzazioneCostruzione1924 Inaugurazione1924 ArchitettoMario Borgato ProprietarioMauro Rota e privato Sito ufficiale Modifica dati su Wikidata · ManualeCoordinate: 45°28′00.35″N 9°09′14.23″E / 45.466765°N 9.153953°E45.466765; 9.153953 Il Teatro Nazionale è un teatro di Milano. Storia S...

MandalawangiDesaNegara IndonesiaProvinsiJawa BaratKabupatenBandung BaratKecamatanCipatatKode pos40754[1]Kode Kemendagri32.17.07.2005 Luas-326.000 HaJumlah penduduk-8.726 SPBU Pertamina di Jalan Nasional Rute 3 yang terletak di Desa Mandalawangi. Mandalawangi adalah Desa di Kecamatan Cipatat, Kabupaten Bandung Barat, Jawa Barat, Indonesia. Batas Wilayah Utara Desa Mandalasari Timur Desa Rajamandala Kulon Selatan Desa Rajamandala kulon Barat Kabupaten Cianjur Referensi ^ Kode Pos K...

Irish sculptor (1946–2006) John BurkeBorn11 May 1946[1]Clonmel, County Tipperary, Ireland[2]Died11 Dec 2006[2]NationalityIrish John Burke (11 May 1946 – 11 December 2006) was an Irish sculptor. Burke studied at the Crawford School of Art and Design in Cork and at the Royal Academy of London.[3] He spent most of his career in the Cork area[4] and for a time taught at Crawford, where his students included Eilis O'Connell and Vivienne Roche.[3&...

Water park on the Gold Coast, Australia Wet'n'Wild Gold CoastSloganBiggest 'n' BestLocationOxenford, Queensland, AustraliaCoordinates27°54′54″S 153°19′04″E / 27.9151076°S 153.3176744°E / -27.9151076; 153.3176744OwnerVillage Roadshow Theme ParksOpened30 September 1984 (1984-09-30)Previous namesCade's County Waterpark(1984–1985)Cade's County Wet'n'Wild(1985–1986)Wet'n'Wild(1986–1997)Wet'n'Wild Water World(1997–2013)Operating seasonAll y...

ХристианствоБиблия Ветхий Завет Новый Завет Евангелие Десять заповедей Нагорная проповедь Апокрифы Бог, Троица Бог Отец Иисус Христос Святой Дух История христианства Апостолы Хронология христианства Раннее христианство Гностическое христианство Вселенские соборы Н...
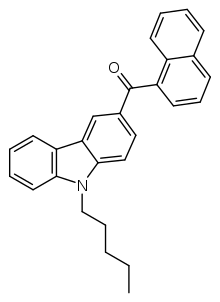
Chemical compound EG-018Legal statusLegal status CA: Schedule II DE: NpSG (Industrial and scientific use only) UK: Under Psychoactive Substances Act Illegal in Japan Identifiers IUPAC name Naphthalen-1-yl-(9-pentylcarbazol-3-yl)methanone CAS Number2219320-91-7PubChem CID118796466ChemSpider30922490UNII5G2788GL5GChemical and physical dataFormulaC28H25NOMolar mass391.514 g·mol−13D model (JSmol)Interactive image SMILES CCCCCN1C2=C(C=C(C=C2)C(=O)C3=CC=CC4=CC=CC=C43)C5=CC=CC=...

Pour les articles homonymes, voir Grand Opéra. L'Opéra Garnier est inauguré le 5 janvier 1875 avec des extraits de La Juive de Jacques Fromental Halévy et des Huguenots de Giacomo Meyerbeer. Jusque-là, les grands opéras étaient donnés dans la salle de la rue Le Peletier, qui fut l'opéra de Paris de 1821 à 1873. Le grand opéra est un genre d'opéra du XIXe siècle, généralement en quatre ou cinq actes, caractérisé par une distribution et un orchestre de grande envergure, d...

Pour les articles homonymes, voir Dodd. Christopher Dodd Portrait officiel de Christopher Dodd (2007). Fonctions Sénateur des États-Unispour le Connecticut 3 janvier 1981 – 3 janvier 2011(30 ans) Prédécesseur Abraham A. Ribicoff Successeur Richard Blumenthal Représentant des États-Unis 3 janvier 1975 – 3 janvier 1981(6 ans) Circonscription 2e district du Connecticut Prédécesseur Robert H. Steele (en) Successeur Sam Gejdenson (en) Biographie Nom de naissan...

Raja SulaemanRaja ke-14 Kerajaan ManilaMasa kekuasaan1571–1575PendahuluRajah MatandaPenggantiAgustin de LegazpiAnakAnak kandung Rajang Bago (Raxa el Vago, dieksekusi oleh pemerintahan Levazarez pada 1574) Doña Maria Laran Anak angkat Agustin de Legazpi (dieksekusi oleh Spanyol setelah terlibat dalam Konspirasi Tondo, c. 1589) Don Gabriel Taumbasan Don Jeronimo Bassi (dieksekusi oleh Spanyol setelah terlibat dalam Konspirasi Tondo, c. 1589) Dalam cerita legenda Prince Suwaboy Da...

German politician (1914–1991) Ewald BucherBucher in 1964Member of the BundestagIn office6 October 1953 – 19 October 1969 Personal detailsBorn(1914-07-19)19 July 1914Rottenburg am NeckarDied31 October 1991(1991-10-31) (aged 77)MutlangenNationalityGermanPolitical partyFDP Ewald Bucher (19 July 1914 in Rottenburg am Neckar, Kingdom of Württemberg – 31 October 1991 in Mutlangen[1]) was a German politician of the FDP.[2] He received a Juris Doctor from the Univ...

Train service in Japan KamuiA 789-1000 series EMU on a Super Kamui / Airport service in January 2009OverviewService typeLimited expressLocaleHokkaidoFirst service22 September 1959 (Kamui)1 October 2007 (Super Kamui)4 March 2017 (Kamui)Current operator(s)JR HokkaidoFormer operator(s)JNRRouteTerminiSapporoAsahikawaDistance travelled136.8 km (85.0 mi)Average journey time1 hour 20 minutesService frequencyHalf-hourlyOn-board servicesClass(es)Standard class onlyTechnicalRolling stock789-1...

Arena in California, United States Bren Events CenterThe BrenFull nameDonald Bren Events CenterLocation100 Bren Event Center DriveIrvine, CA 92612Coordinates33°38′57″N 117°50′49″W / 33.64917°N 117.84694°W / 33.64917; -117.84694OwnerUniversity of California, IrvineOperatorUniversity of California, IrvineCapacity4,984 (for basketball)5,430 (for concerts)5,608 (maximum)SurfaceHardwoodConstructionBroke ground1984OpenedJanuary 8, 1987Construction cost$14 million...

Liga A LituaniaNegaraLituaniaKonfederasiUEFADibentuk1991Jumlah tim10 (sejak 2021)Tingkat pada piramida1Degradasi keI LygaPiala domestikPiala Sepak Bola Lituania Piala Super LituaniaPiala internasionalLiga Champions Liga EropaJuara bertahan ligaFK Panevėžys (gelar ke-1) (2023)Klub tersuksesFK Žalgiris (10 gelar)Televisi penyiarDELFI TVInit TV[1]Situs webwww.alyga.lt A lyga 2024 Liga A Lituania (Bahasa Lithuania: A Lyga) adalah liga sepak bola antar klub pada tingkat tertinggi di Lit...

Protokol Opsional Konvensi mengenai Hak-Hak Penyandang Disabilitas partai negara negara yang menandatangani, namun tak meratifikasi negara yang tak menandatanganiDirancang13 Desember 2005Ditandatangani30 Maret 2007LokasiNew YorkEfektif3 Mei 2008Syarat10 ratifikasi dan pemberlakuan Konvensi Hak-Hak Penyandang DisabilitasPenanda tangan93Pihak94PenyimpanSekretaris-Jenderal Perserikatan Bangsa-BangsaBahasaArab, Tionghoa, Inggris, Prancis, Rusia dan Spanyol Proto...

American mathematician Edward Burr Van Vleck Edward Burr Van Vleck (June 7, 1863 – June 2, 1943)[1] was an American mathematician. Early life Van Vleck was born June 7, 1863, Middletown, Connecticut. He was the son of astronomer John Monroe Van Vleck, he graduated from Wesleyan University in 1884, attended Johns Hopkins in 1885–87, and studied at Göttingen (Ph.D., 1893). He also received 1 July 1914 an honorary doctorate of the University of Groningen (The Netherlands).[2]...

Catholic Church ecclesiastical community Part of a series onParticular churches sui iurisof the Catholic Church Latin cross and Byzantine Patriarchal cross Particular churches are grouped by liturgical rite Alexandrian Rite Coptic Ethiopian Eritrean Armenian Rite Armenian Byzantine Rite Albanian Belarusian Bulgarian Croatian and Serbian Greek Hungarian Italo-Albanian Macedonian Melkite Romanian Russian Ruthenian Slovak Ukrainian East Syriac Rite Chaldean Syro-Malabar Latin liturgical rites La...
هذه المقالة بحاجة لصندوق معلومات. فضلًا ساعد في تحسين هذه المقالة بإضافة صندوق معلومات مخصص إليها. رحلات كولمبوس الأربعة. الخط الأزرق: الرحلة الأولى. الخط الأحمر: الرحلة الثانية. الخط الأخضر: الرحلة الثالثة. الخط البرتقالي: الرحلة الرابعة. قاد المستكشف الإيطالي كريستوفر كو�...